
By Dr. Tracy Tranchitella, ND
Acute inflammation has a purpose and occurs when we are injured or sick and need to mobilize an efficient immune response to heal an injury or attack an infection. When all goes well, the response of the immune system is swift and complete. The job is done, the immune cells recede, and the clean-up crew disposes of the debris. Chronic inflammation, on the other hand, tends to linger without purpose or resolution. It may be the leftover remnant of an acute inflammatory process that never fully resolved, or it may exist as its own process triggered by low-level infections, food sensitivities, toxin exposure, metabolic dysregulation, and autoimmune processes.
Addressing the cause is the first and most important step and can often be the most challenging as there may be several promoters of ongoing inflammation. While we sleuth our way through what can be a tedious process of discovery, it is important to dampen the inflammation, reduce damage and oxidative stress from the inflammatory process, and support a healthy resolution.
What’s New in the World of Essential Fats
Essential fats have been studied for several decades and entire books have been written on the subject, yet we are still learning about the role these fats play in regulating inflammation. Within the study of essential fats, some new players have emerged—the specialized pro-resolving mediators or SPMs. These are important metabolites of omega-3 fats and arachidonic acid that, as the name implies, specifically help to resolve inflammation. So how do they do that, where do they come from, and how can we get some?
Omega-3 & Omega-6 Fatty Acid Sources
Our main sources of essential fats are the omega-3 and omega-6 fatty acids. These are polyunsaturated fatty acids and are considered essential because we must get them through our diet. The parent fatty acid of omega-6 fats is linoleic acid, and the parent fatty acid of omega-3 fats is alpha-linolenic acid. Through enzymatic activity, each of the parent fatty acids can be converted to other omega-6 or omega-3 fatty acids or we can get them from specific foods or supplements. The process of converting one fatty acid to another requires the presence of specific enzymes. Both omega-6 and omega-3 fats use the same enzymes to convert one fat to another so the presence of adequate omega-3 fats can competitively inhibit the production of the omega-6 fatty acids, which can be a good thing as the omega-3 fats tend to be anti-inflammatory. Genetics and aging can have an inhibitory effect on enzyme production rendering those conversion pathways less effective so getting a variety of essential fats from foods and supplements is often recommended.
The three main omega-3 fatty acids and their sources are:
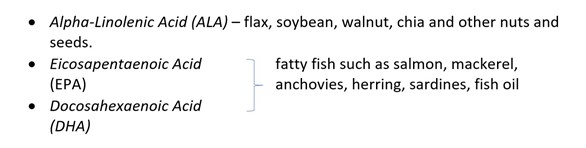
There are four types of omega-6 fats that are abundantly available in many of the foods that we eat, making it much easier to get our fill of omega-6 fats over omega-3.
The four omega-6 fatty acids and their sources are:
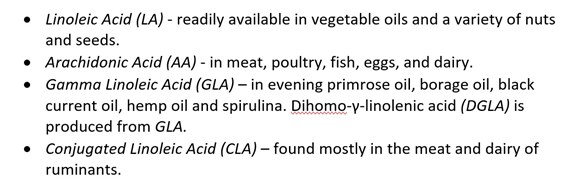
Omega-3 and omega-6 fats are structurally different, so they behave differently. As these fatty acids are metabolized through enzymatic pathways, they produce specific products that may promote or inhibit inflammation.
Wikipedia contributors. (2022, March 9). Eicosanoid. In Wikipedia,
The Free Encyclopedia. Retrieved May 24, 2022.
Eicosanoids
Prostaglandins, leukotrienes, and thromboxanes are eicosanoids produced from the enzymatic breakdown of arachidonic acid (omega-6), EPA (omega-3) and DGLA (omega-6). Eicosanoids are derived from fatty acids that are 20 carbon units in length and function as signaling molecules that promote or inhibit inflammation. Arachidonic acid produces more inflammatory eicosanoids while EPA and DGLA produce eicosanoids that are less inflammatory. The designation of pro-inflammatory and anti-inflammatory may be an over-simplification as each eicosanoid exerts a specialized effect dependent upon the tissues in which they are produced and where they exert their activity. Inflammation is a necessary part of the immune response and is not always a negative. We need both inflammation and resolution as part of the immune response just as we need the gas and the brake in a vehicle—both serve a purpose.
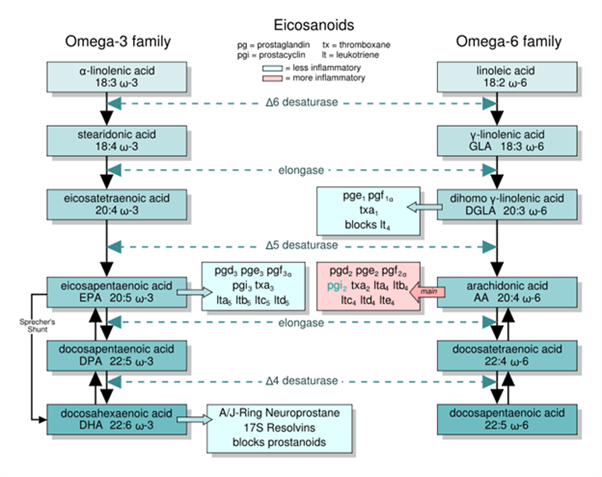
Specialized Pro-Resolving Mediators
Another component of fatty acid breakdown are the specialized pro-resolving mediators (SPMs). These are lipid mediators that help to resolve inflammation and restore normal cellular function following an inflammatory episode. SPMs are produced from arachidonic acid, EPA, and DHA. Resolvin, maresin and protectin are produced from EPA and DHA, and lipoxin is produced from arachidonic acid. SPMs are further designated as E-series if they are derived from EPA, and D-series if they are derived from DHA. Lipoxin is the only SPM produced from an omega-6 fatty acid and functions as the lead family of pro-resolving mediators to reduce inflammation and restore tissue integrity.
Chiang N, Serhan CN. Essays in Biochemistry. 2020;64(3).
How Do SPMs Resolve Inflammation?
SPMs stimulate macrophage-mediated clearance of the debris that is produced as part of an immune response. Neutrophils that have engulfed a pathogen will undergo apoptosis. This signals macrophages to engulf the spent neutrophils and carry them into the lymph system for clearance. Efferocytosis is the process of removing post-inflammatory cellular debris by macrophages and is key to supporting the resolution of inflammation. If macrophages are not recruited to the scene, the dying neutrophils release their cell contents, which signals that tissue damage has occurred. If damage is occurring in the tissues, more immune cells are recruited to the site and inflammation continues rather than resolves.
The acute inflammatory process initiated towards a pathogen should be self-limiting with the return of the tissue to a pre-inflammatory state. SPMs participate in the process of resolution of the inflammatory state, which allows tissues to begin the process of repair and regeneration rather than slipping into a state of chronic inflammation.
Sources of SPMs – What You Make and What You Take
Supplementing with omega-3 fats has been a recommendation of both alternative and conventional medical practitioners for decades. The pathways that the omega-3 and omega-6 fats take, and the enzymes involved in their conversions are well-mapped out. We have a clear understanding of which eicosanoids promote inflammation and which reduce inflammation, and it seems clear that if we get enough omega-3 fats in our diet, we should produce enough SPMs. But that might not always be the case.
Enzymatic production of SPMs from fish oil has been identified as one of the bioactive processes that contributes to the anti-inflammatory effects. Conversion of EPA and DHA to SPMs can be a slow and complex process in which success is dependent upon several factors. If the enzymes necessary for the conversion of fish oil are insufficient, we cannot produce the SPMs and benefit from their effects. The enzymes necessary to support the conversion process have roles in other pathways and may be diverted to other uses, leaving the production of SPMs deficient. Aging, toxic overload, poor diet, stress, genetics, and lack of sleep can also complicate this process via reduction of biosynthetic potential.
Ultimately, the formation of SPMs is determined by the presence of omega-3 fats in the diet, the ability to absorb fats, and availability of the necessary enzymes to create SPMs. If any one of those components is missing, the benefits of supplementing with fish oil are greatly reduced. Several supplement companies have developed fish oil products using a patented fractionation process that creates immediate precursors to SPMs, which helps get around all the factors that may limit their availability.
Benefits of SPMs
Glucocorticoids, aspirin, other non-steroidal anti-inflammatory drugs, and more recently, biologics that inhibit specific mechanisms of inflammation all function through the inhibition of inflammatory pathways. Supplementing directly with SPMs can support the resolution of acute inflammation, as well as addressing chronic inflammatory processes without compromising a healthy immune response. Acute inflammation is necessary; however, inflammation that does not resolve can perpetuate tissue damage and advance an ongoing disease process.
SPMs have proven useful in supporting recovery from lung infections, surgery, head trauma, and stroke. Additionally, SPMs show efficacy in helping to resolve cardiovascular inflammation, asthma, inflammatory bowel disease, sepsis, periodontal disease, and injury to muscles and bone. Combining supplementation of SPMs with specific antioxidants and phytonutrients that provide protection from oxidation is ideal in addressing ongoing inflammation. Quercetin, resveratrol, turmeric, epigallocatechin gallate from green tea, vitamins C and E along with a diet rich in vegetables can reduce oxidative stress and reduce tissue damage from an ongoing inflammatory process.
While we want the immune system to do its job in supporting the clearance of pathogens and allowing us to heal from injury, the resolution of inflammation is also an important component of a healthy immune response. Inflammation can be a contributing factor in the development of countless chronic diseases and can interfere with recovery from an acute illness. SPMs can support the body’s efforts to bring a complete resolution to the inflammatory process, allowing tissues to heal and return to normal function.
ZRT Testing: The Link to Inflammation
Inflammation can be an underlying process in any chronic disease. Hormone imbalances, hypothalamic-pituitary-adrenal axis dysfunction, metabolic syndrome, insulin resistance, cardiovascular disease, and autoimmune conditions can contribute to or result from chronic inflammation. Screening for functional imbalances in sex, thyroid and adrenal hormones can provide some insight regarding underlying contributors to general inflammation. Measuring cholesterol, triglycerides, HgA1C and fasting insulin in a dried blood spot is a convenient way to screen for elevated blood lipids, poor blood sugar control, and insulin resistance. These markers can be indicative of developing cardiovascular disease and metabolic disorders, which all contribute to and are worsened from unresolving inflammation. Lastly, ZRT measures high-sensitivity C-reactive protein, which increases in the blood with inflammation and infection, and is often used as a predictive tool for the development of cardiovascular disease.
Related Tests

Resources
1. Basil MC, Levy BD. Specialized pro-resolving mediators: endogenous regulators of infection and inflammation. Nat Rev Immunol. 2016;16(1):51-67.
2. Rosenthal MD, Patel J, Staton K, et al. Can specialized pro-resolving mediators deliver benefit originally expected from fish oil? Curr Gastroenterol Rep. 2018;20(9):40.
3. The spectrum of pro-resolving mediators (PRMs). Big Bold Health Professional. 2021. Accessed May 20, 2022.
4. Silverman R. Specialized pro-resolving mediators: a new tool for resolving inflammation. 2017. Accessed May 20, 2022.
