
By Dr. Zane Hauck, ZRT Laboratory
Growing up, I never thought of myself as a runner, or really a good athlete in general. I played every sport possible as a kid, but I was never great and didn’t play high school sports. As an adult, I started playing team sports again and eventually was convinced to run a 5k. I ended up running the Warrior Dash and enjoyed it, so I continued doing 3.2-mile training runs. For the rest of my 20s I continued running 5k races with friends and played volleyball, softball, and some casual intramural sports, but was there more to my athletic prospects?
Going the Extra Mile
In 2015, my wife came up with the crazy idea of running the Chicago Triathlon. Running was fun and all, but the prospect of doing multiple sports in one race really appealed to me. We trained together, swimming in Lake Michigan and running and biking on the lakefront trail. In June of 2016 I completed my first sprint distance triathlon and I instantly wanted to do it again! However, as life happens, triathlons got put on hold. After our first child was born, my wife promptly set a goal to complete another triathlon before she was a year post-partum and did 2 sprint triathlons in 2018. My next goal was an Olympic distance triathlon, which I completed in 3:12:58. Two weeks later I did another Olympic tri and my worst nightmare came true as I got a flat tire on my bike 0.25 miles in. I managed to change the tire on the side of the road, but it set the tone for a rough day.
Since starting at ZRT I started tracking my hormones and studying how they change and affect my training and performance. Having another tool in my training toolbox has improved my performance by being able to optimize my workload and recovery balance. Never in my life did I think I would enjoy running, let alone be as much of an athlete as I am. I am currently training for a half-marathon between triathlon seasons and have used the data from my hormone tracking to get my times down to under 8 minutes per mile.
Laboratory Medicine and Athletics – Which Hormones are Involved?
Laboratory medicine in sport is an important preventative and protective science, fundamental for evaluating the condition of an athlete. The balance between workload and recovery is important for athletes to prevent injury while maintaining the highest level of competition. This balance can be monitored and optimized using laboratory medicine, particularly through the prevention of overtraining. It has been established that healthy athletes have adaptations to their hormonal conditioning [1].
Thyroid hormones regulate energy metabolism and can influence energy processes during physical exercise [2]. Thyroid hormones are also important regulators of cardiac function, protein synthesis, and calcium homeostasis. Hypothyroidism causes a decrease in athletic performance and capacity while hyperthyroidism can also cause a decrease in athletic performance through weight loss and tachycardia [2]. Analysis of thyroid hormone levels can help prevent issues and allow an athlete to reach optimal athletic performance.
Steroid hormones endogenously produced by the body are important in maintaining energy stores, building muscle, increasing oxygen capacity, decreasing fatigue and recovery time, and optimizing hand-eye coordination. The main hormone responsible for these effects is testosterone, the main sex hormone in males. Testosterone is found in both men and women. Progesterone, estradiol, and cortisol are also important hormones regarding athletic performance and must be balanced along with testosterone. Progesterone helps maintain proper activity of the thyroid, which can help increase energy availability and helps keep inflammation in check. Estradiol is the main sex hormone in women, but also important in men as well and is responsible for controlling inflammation, reducing muscle damage, and helping break down fat for fuel. Cortisol and aldosterone help in regulating metabolism, blood sugar, and water/salt balance. Excess cortisol can cause muscle breakdown and fatigue.
Now that you know about the hormones that affect you while exercising, how can you use this information to increase athletic performance? There are many ways to monitor these hormones that will give insight into whether you have the correct diet, are overtraining, or possibly have other health issues.
Hormones and Overtraining Syndrome
Overtraining syndrome (OTS) happens when the balance between training and recovery get out of sync. This is a result of the body not being able to return to homeostasis after physical exercise. Recovery is just a short way of saying the regenerative process of re-establishing homeostasis. If exercise continues before recovery completes, an accumulation of fatigue occurs. At early stages of OTS, often called overreaching, only fatigue and decreased performance present themselves, which can be overcome with a longer recovery period. If OTS continues, more long-term problems occur that change the physiology of the body and can take months to overcome [3]. Gonadal and adrenal steroids have been used as biomarkers of overtraining in athletes and can be used to assess whether an athlete is in early or late stage OTS [4].
Estradiol and testosterone levels and their ratio have shown to be diagnostic in OTS [5]. Testosterone is shown to have a slight increase at the start of exercise but declines thereafter [3]. Normally, testosterone levels rebound overnight with rest, but after severe exercise this rebound can be delayed [3,6]. However, in trained endurance athletes, basal levels of total testosterone and free androgens are decreased over time [7,8]. This decrease in testosterone can increase the susceptibility to OTS as well as decrease sperm quality [8]. This can be assessed by looking at sex hormone binding globulin (SHBG), which binds free steroids in the blood and keeps them bound and soluble allowing for transport through the blood vasculature. Increasing SHBG in response to the lowering levels of testosterone over time can be indicative of OTS [6]. Overtraining in female athletes can lead to low estrogen levels and menstrual disorders [4]. Dehydroepiandrosterone (DHEA) levels are associated with muscular enzyme activity and are associated with muscular traction during exercise [2]. Cortisol is increased during high-intensity exercises in many sports but rapidly decreases after exercise and is not suitable for monitoring for OTS.
Growth hormone (GH) levels are higher in athletes than in sedentary people, but with no increase in insulin-like growth factor I (IGF-1) [1]. Usually the liver secretes IGF-1 based on how much GH it receives, which is secreted from the pituitary gland. This is important because IGF-1 is the mediator of GH activity, stimulating systematic growth, whereas GH has very specific individual actions [9]. Increases in GH in athletes help by promoting more targeted growth in areas that are important for athletes. These effects include calcium retention, direct muscle mass growth, increased protein synthesis, enhanced gluconeogenesis for energy production, and increased conversion of T4 to T3, the active thyroid hormone [9].
A surprising find is that athletes have a prevalence of vitamin D insufficiency, despite the fact they can spend a lot of time outside training [1,10]. This insufficiency is due to the expression of vitamin D receptors in muscles causing a decrease in circulating vitamin D due to high muscle activity [1,10]. In addition to its role in bone health, vitamin D is also important in immune regulation, protein synthesis, inflammatory response, cell growth, and skeletal muscle strength and function [11]. One of the main clinical indicators of vitamin D deficiency is muscle weakness and myopathy [11]. A few studies showed that vitamin D supplementation increased musculoskeletal performance especially with regard to vertical jump height, as well as hand strength, aerobic power and capacity, and sprinting ability [12]. Vitamin D also plays a big role in muscle regeneration following injury [12].
Catecholamines can also be effective in measuring the degree of OTS [8]. Catecholamines are neurotransmitters that include dopamine, norepinephrine (noradrenaline) and epinephrine (adrenaline). Dopamine is involved in reward and pleasure in the brain and as a vasodilator in the rest of the body. Norepinephrine is part of the sympathetic nervous system (fight-or-flight response) and is involved in alertness, focus, and readiness. Epinephrine is important in receptor-dependent vasoconstriction, which allows for greater cardiac output. The surge of adrenalin at the start of athletic activity increases alertness and boosts the heart rate allowing for more available oxygen for working muscles. Studies show that during recovery periods before competitions, norepinephrine levels typically are lower in well-trained athletes than in over-trained athletes [13]. Monitoring norepinephrine levels during training or when athletes feel as if they aren’t getting the most out of their workouts can help identify the early stages of OTS.
How Does Menstruation Affect Women Athletes?
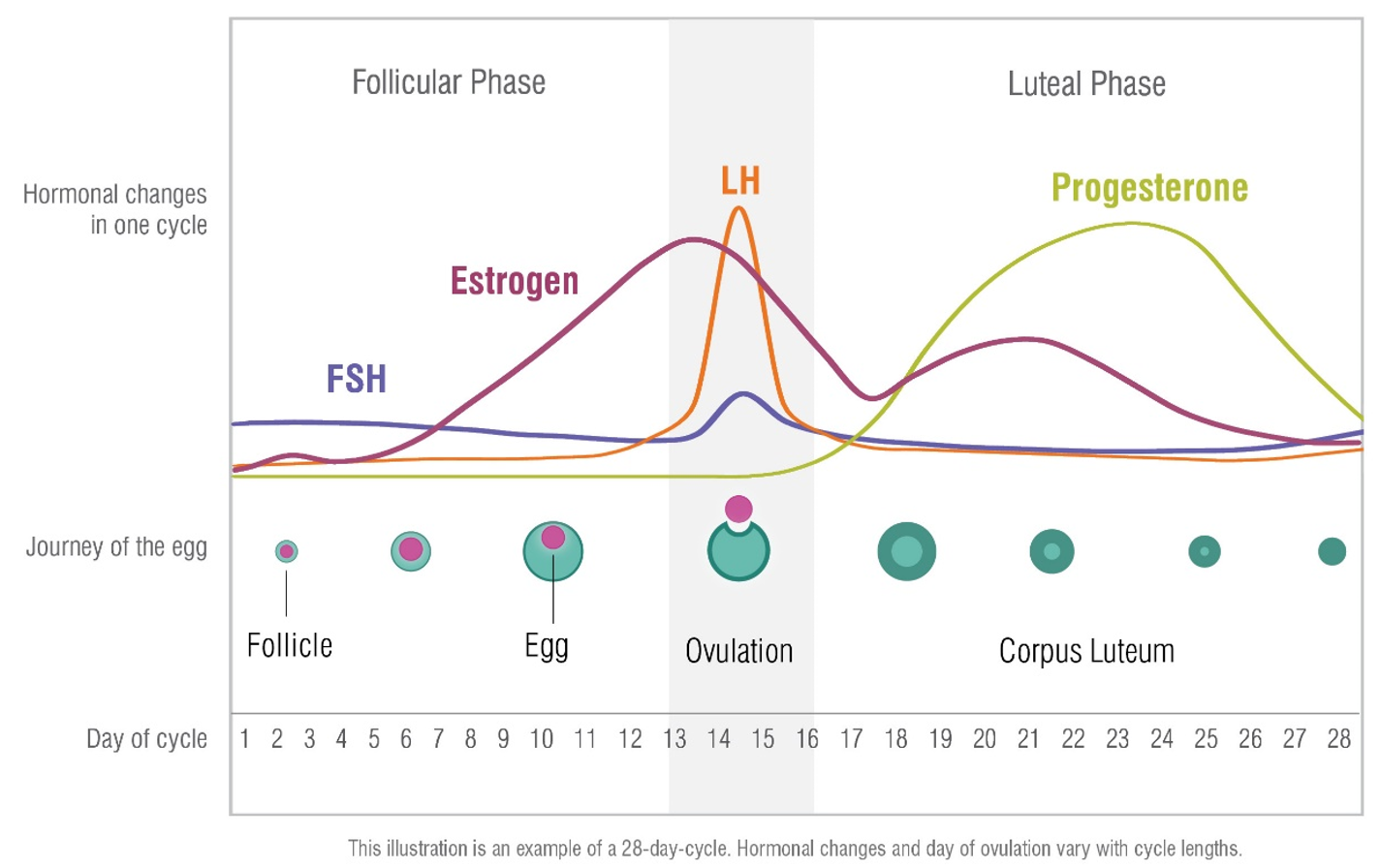
Men and women vary in many ways when it comes to sports and exercise, but the biggest difference, which can have far reaching effects, is the cyclical change in hormones that occur in women throughout the menstrual cycle. Almost half of all women believe their menstrual cycle has a negative impact on their training and performance [14]. Research is being conducted to optimize female training and performance while decreasing injury with regard to menstruation status. Women use carbohydrates more efficiently in the follicular phase and are better at using fats and amino acids in the luteal phase [14]. While exercise is touted to have many beneficial effects, intense exercise can lead to problems if not monitored closely. Intense exercise has an effect on the hypothalamic-pituitary-gonadal axis as well as inducing a state of energy deficiency which can inhibit the release of gonadotropin releasing hormone (GnRH) and luteinizing hormone (LH), both of which direct the body in how much hormone to make. Lactate levels in the blood are lower during physical activities in the luteal phase when progesterone is high, delaying the onset of fatigue [15,16].
Energy deficiency or availability (EA) is one of the pillars of the female athlete triad which explains the interrelationship between EA, menstrual function, and bone mineral density (BMD) and their clinical manifestation in eating disorders, osteoporosis, and amenorrhea [17]. These effects can be ameliorated by adjusting training protocols to be more in sync with the menstrual cycle, or through the use of oral hormonal contraceptives. The US Women’s National Soccer Team tracked their cycles and tailored their workouts to coincide with their menstruation status. Research suggests strength training is more advantageous during the first half of the cycle due to better recovery and adaptation of the body [14]. However, due to higher estrogen levels, the risk of injury can be higher during this time as well. Again, these effects are only present in intense exercise or sports that necessitate low weight. Moderate exercise is beneficial for both men and women.
Fluctuations in hormones can increase the risk of certain types of injuries during different phases of the menstrual cycle. One study found that anterior cruciate ligament (ACL) injuries are more common in the follicular and ovulatory phases [14,18]. This is unique to ligaments, specifically the ACL because the ACL has estrogen receptors, which inhibit synthesis of type I collagen synthesis [19]. Another study found that concussions were more likely and the symptoms more severe during late luteal/early menstruation when both estrogen and progesterone are at their lowest levels [20]. Estrogen and progesterone have both shown neuroprotective effects as well as modulating the inflammatory response to injury. Progesterone has a thermogenic effect, raising basal body temperature by around 0.5°C, which can lead to a thermoregulatory disadvantage for female athletes in extreme heat and humidity during the luteal phase [18].
Iron deficiency is another issue that can plague female athletes, as well as men, and is one of the most common deficiencies in sports [21]. Female athletes are particularly at risk due to the loss of iron during menstrual bleeding. Athletes require more iron to build up their red blood cells due to the requirements of regular exercise. Athletes require higher aerobic output and one of the physiological adaptations to promote delivery of oxygen-rich blood to muscles is to increase blood volume or red cell mass along with increased cardiac size and function and enhanced off-loading of oxygen at the tissue level [21]. Iron is also an important factor in the electron transport chain which is one of the main producers of energy in the body [21]. Iron is essential for thyroid hormone synthesis (2). Iron is also important in brain development and cognition. Deficiencies can lead to impairment of concentration, motivation, and decision-making [21]. The International Olympic Committee (IOC) recommends periodic testing of serum ferritin and hemoglobin [21] to assess iron status.
Post-menopause athletes don’t have to worry about the cyclical nature of their hormones, but they do have to be aware of the lower levels of hormones. While exercise is very important for post-menopausal women to help control the issues that arise from lower hormone levels such as muscle loss and osteoporosis, it will be important to monitor hormone levels in case hormone replacement therapy (HRT) may be needed. Exercise has been shown to increase muscle mass, help prevent bone density loss, decrease risk of coronary heart disease, and may help reduce hot flashes [22].
Testing Your Hormones and Nutrients to Improve Your Performance
Now that you know how your hormones and nutritional status play into athletic performance, what can you do about getting tested? Most of the parameters I discussed can be tested in a clinical laboratory like ZRT. It is important to get a general health baseline of your hormonal and nutritional status before beginning an intense training regime. This will allow you to address areas of need before they have a chance to become a problem and throw you into OTS. ZRT has simplified hormone testing by allowing you to noninvasively collect various body fluids that can be used for hormone testing. Here is an outline of a basic testing option I recommend with some add-on options.
Start with the Comprehensive Female Profile I / Comprehensive Male Profile I. This panel tests saliva for the important parent hormones as well as dried blood spot (DBS) for thyroid hormones. I would add-on vitamin D in DBS. I like looking at saliva for the steroid hormones because saliva gives you a better picture of what the cells are seeing rather than what is just being circulated, bound and unbound, throughout the body.
I would recommend getting a baseline test before beginning a training regimen, but if you have already begun training, it would be best to test during one of the recovery periods to get values as close to baseline as possible. I would consider retesting periodically throughout your training program or anytime you feel like you are “hitting the wall” to help understand why this is happening to allow for changes in training to prevent it in the future.
Related Tests
Fitness Metrics Profile
References
[1] Luger A, et al. Acute Hypothalamic-Pituitary-Adrenal responses to the stress of treadmill exercise. N Engl J Med. 1987;316:1309-1315.
[2] Lombardo B, et al. Laboratory medicine: health evaluation in elite athletes. Clin Chem Lab Med. 2019;March 5:ePub.
[3] Kuipers H, and Keizer HA. Overtraining in elite athletes. Sport Med. 1988;6:79-92.
[4] Cadegiani FA, et al. Basal hormones and biochemical markers as predictors of overtraining syndrome in male athletes: the EROS-BASAL study. J Athl Train. 2019;54:ePub.
[5] Cadegiani FA. Et al. Novel insights of overtraining syndrome discovered from the EROS study. BMJ Open SP Ex Med. 2019;5:1-11.
[6] Urhausen A, et al. Blood hormones as markers of training stress and overtraining. Sport Med. 1995;20:251-276.
[7] Maimoun L, et al. Testosterone is significantly reduced in endurance athletes without impact on bone mineral density. Horm Res. 2003;59:285-292.
[8] Lucía A, et al. Reproductive function in male endurance athletes: sperm analysis and hormonal profile. J appl physiol. 1996;81:2627-2636.
[9] Holt RIG, et al. The use and abuse of growth hormone in sports. Endo Review. 2019;40:1163-1185.
[10] Lanteri P, et al. Vitamin D in exercise: physiologic and analytical concerns. Clin Chim Acta. 2013;415:45-53.
[11] Alimoradi K, et al. Efficacy of vitamin D supplementation in physical performance of Iranian elite athletes. Int j prev med. 2019;10:100
[12] Wiciński M, et al. Impact of vitamin D on physical efficiency and exercise performance – A review. Nutrients. 2019;11:2826.
[13] Hooper SL, et al. Hormonal responses of elite swimmers to overtraining. Med Sci in Sport and Excise. 1993;25:714-747.
[14] Oleka CT. Use of the menstrual cycle to enhance female sports performance and decrease sports-related injury. J Ped Adol Gyn. 2019; pii:S1083-3188(19)30319-5.
[15] Lagowska K, et al. Testosterone concentrations in female athletes and ballet dancers with menstrual disorders. Euro j sport sci. 2016;16:490-497.
[16] Orio F, et al. Effects of physical exercise on the female reproductive system. Minerva Endo. 2013;38:305-319.
[17] Weiss Kelly AK, et al. The female athlete triad. Pediatrics. 2016;137:e20160922.
[18] Constantini NW, et al. The menstrual cycle and sport performance. Clin sports med. 2005;24:e51-e82.
[19] Balachandar V, et al. Effects of the menstrual cycle on lower-limb biomechanics, neuromuscular control, and anterior cruciate ligament injury risk: a systematic review. Muscles ligaments tendons J. 2017;7(1):136-146.
[20] La Fountaine MF, et al. Preliminary evidence for a window of increased vulnerability to sustain a concussion in females: A brief report. Front neurol. 2019;10:691.
[21] Pedlar CR, et al. Iron balance and iron supplementation for female athlete: A practical approach. Euro j sport sci. 2018;18:295-305.
[22] Shangold MM, et al. Exercise and menopause. Physician sport med. 1998;26(12):45-52.
