
In this blog, I want to focus mainly on how cannabis can affect your hormones, primarily through the pituitary, thyroid, and adrenal glands, and the reproductive system.
While cannabis is being legalized in more and more states, both the adverse and beneficial effects of its use are starting to be better understood. The active compound in cannabis, THC (tetrahydrocannabinol) is widely known to have effects on the brain, producing the “high” that many users are seeking. However, the other more adverse effects cannabis can have on the body are less widely known.
The Endocannabinoid System (ECS) and How It Works
Endocannabinoids are molecules naturally produced in the body in small amounts that act on cannabinoid receptors and play important roles in various processes. There are 2 types of cannabinoid receptors in the body, CB1 and CB2, and a few orphan receptors that also bind with the endocannabinoids. These are the same receptors that THC binds and activates (and CBD, which I won’t cover here). The ECS is involved in regulating fertility, pregnancy, appetite, pain-sensation, mood, memory, energy balance, homeostasis, and the immune system. The ECS is also responsible for “runner’s high” through spikes in endocannabinoids circulating in the blood to the brain, where it is involved in locomotor activity through interactions with the cerebellum and affects the reward center of the brain through transduction of dopamine release.
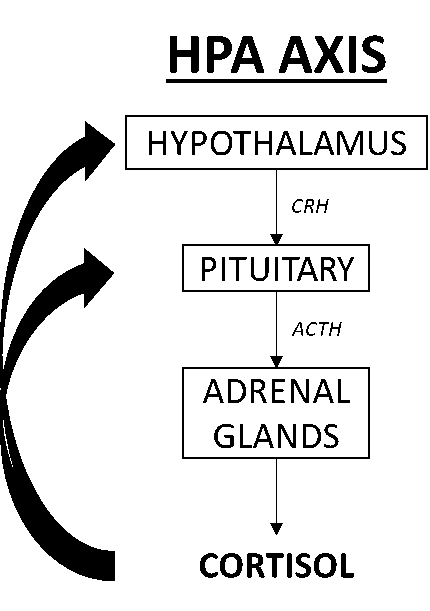
Acute high cortisol is essential for optimal health, since cortisol helps control blood sugar levels, regulates metabolism, reduces inflammation, controls salt and water balance which influences blood pressure, and assists with memory formation. However, persistent high cortisol caused by excessive stressors will eventually have a negative impact on health. Prolonged release of high levels of cortisol reduces the sensitivity of the negative feedback loop that controls cortisol levels and reduces its effectiveness [1].
It has been shown that THC increases circulating cortisol levels after use [2][3]. For infrequent cannabis users, this increase in cortisol can cause increases in blood pressure and anxiety [4]. In long-term users, sustained increase of cortisol blunts the body’s natural reactions to changes in cortisol and can affect a woman’s libido and menstrual cycle [3][4]. Long-term use also has the potential to blunt the morning spike of cortisol, referred to as the Cortisol Awakening Response (CAR). Upon waking, cortisol levels spike, slowly declining throughout the day. This spike of cortisol is important in facilitating the body to wake up. If this spike is blunted, it becomes difficult to shake off sleep and function normally.
Cannabis’s Effects on the Hypothalamus-Pituitary-Thyroid (HPT) Axis
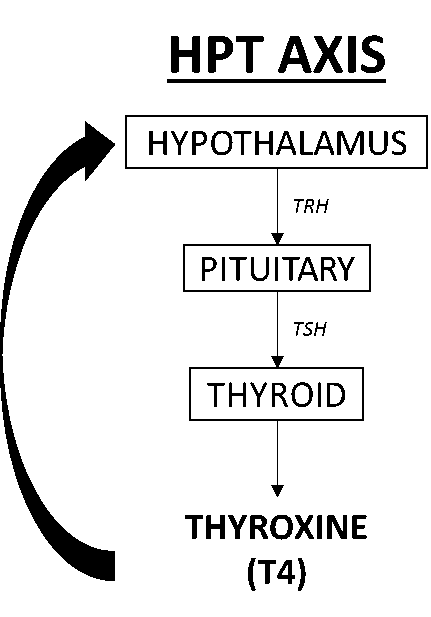 The HPT axis is responsible for maintaining metabolic rate, heart and digestive functions, muscle control, brain development, and bone health. Briefly, the hypothalamus releases thyrotropin-releasing hormone (TRH) which then binds with the pituitary gland, stimulating the release of thyroid-stimulating hormone (TSH). TSH then stimulates the release of thyroxine (T4) and triiodothyronine (T3) from the thyroid. T4 exerts a negative feedback with the hypothalamus to regulate how much is circulating in the bloodstream.
The HPT axis is responsible for maintaining metabolic rate, heart and digestive functions, muscle control, brain development, and bone health. Briefly, the hypothalamus releases thyrotropin-releasing hormone (TRH) which then binds with the pituitary gland, stimulating the release of thyroid-stimulating hormone (TSH). TSH then stimulates the release of thyroxine (T4) and triiodothyronine (T3) from the thyroid. T4 exerts a negative feedback with the hypothalamus to regulate how much is circulating in the bloodstream.
THC inhibits secretion of TSH from the pituitary gland mostly through regulation of TRH release in the hypothalamus [5][6]. This effect is dose-dependent, meaning the more you consume, the more it depresses the TSH levels [5][6]. This decrease in TSH levels causes a decrease in synthesis of T4 and T3 in the thyroid gland and consequent lower circulating T4 and T3 levels [5][6]. Low circulating T4 and TSH levels can lead to symptoms of pituitary hypothyroidism including fatigue, weight gain, cold intolerance, depression, decreased libido, and abnormal menstrual cycles.
The HPG axis oversees the body’s functionsrelated to reproductive health and regulates our hormones to maintain optimal function and health of all tissues throughout the body (brain, connective tissue, cardiovascular, reproductive organs, immune system, etc.). Briefly, the hypothalamus secretes gonadotrophin-releasing hormone (GnRH) which stimulates the pituitary to secrete follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
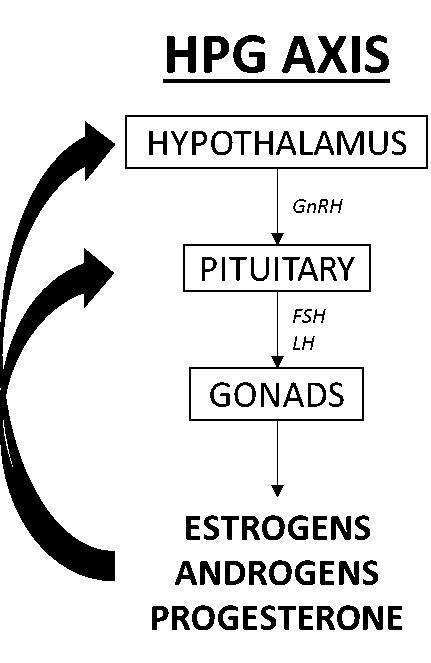
FSH and LH are important in regulating gonadal function in both sexes. In women, FSH and LH are important for pubertal development and ovarian function and play an important role during the menstrual cycle. In men, FSH is essential to the function of the testes and their production of sperm (spermatogenesis) and LH stimulates the production of testosterone. Cannabis use directly impacts many parts of the HPG axis. THC indirectly decreases the secretion of GnRH by the hypothalamus through regulation of the neurotransmitters glutamate and gamma-aminobutyric acid (GABA) [7][8], and through the transduction of dopamine, which is shown to decrease GnRH signaling [9]. In women, THC inhibits folliculogenesis, the maturation of the ovarian follicle, and ovulation, through the regulation of cellular energy produced in the mitochondria, cAMP [7]. During ovulation, the body releases a surge of endocannabinoids in the ovary; excess cannabinoids from cannabis consumption can disrupt the ovulatory surge and lead to an irregular cycle [7][8]. THC also inhibits steroidogenesis by preventing the conversion of pregnenolone to progesterone [7]. In men, THC has been shown to decrease sperm count, reduce serum testosterone and LH levels, reduce sperm motility, and inhibit the processes needed to facilitate sperms’ ability to achieve conception [7][10][11]. These effects can lead to a decrease in fertility in both men and women, but fertility can return with cessation of use.
In summary, chronic cannabis consumption can have effects on the adrenal, thyroid, and reproductive systems that can potentially affect energy, behavior, and reproductive health. Fortunately, after stopping long-term, chronic use, the body can restore normal function, hopefully mitigating these effects. THC also has an impact on the developing fetus so stopping cannabis use while trying to conceive will help both you and your developing child [12].
In this blog, I only addressed the THC component of cannabis. In a future blog, I will address cannabidiol (CBD), the other major cannabinoid without the psychotrophic effects of THC, that is showing great promise as a medicine.
If you are a habitual cannabis user and your energy level and sex-drive are lackluster, it may be wise to periodically test your levels of adrenal hormones (cortisol, DHEA-S), sex hormones (estradiol, progesterone, and testosterone), and thyroid hormones (T4, T3, TSH, TPOab) to make sure THC isn’t blunting your edge. Simple and convenient saliva and blood spot tests can help determine if cannabis use is impacting your overall health.
Source:By Zane Hauck, PhD of ZRT Laboratory.
References
[1] Hill MN, et al. Endogenous cannabinoid signaling is essential for stress adaptation. Proc Natl Acad Sci USA. 2010;107:9406-11.
[2] Hilliard CJ, et al. Endocannabinoid signaling and the hypothalamic-pituitary-adrenal axis. Compr Physiol. 2018;7: 1-15.
[3] Ranganathan M, et al. The effects of cannabinoids on serum cortisol and prolactin in humans. Psychopharmacology. 2009;203:737-44.
[4] Cservenka A, et al. Cannabis use and hypothalamic-pituitary-adrenal axis functioning in humans. Front. Psychiatry 2018;9:472.
[5] Malhotra S, et al. Effect of cannabis use on thyroid function and autoimmunity. Thyroid. 2017;27:167-73.
[6] Hillard CJ, et al. The effects of Δ9-Tetrahydrocannabinol on serum thyrotropin levels in the rat. 1984;20:547-50.
[7] Walker OS, et al. The role of the endocannabinoid system in female reproductive tissue. J Ovarian Res. 2019;12:3.
[8] Brown TT, Dobs AS. Endocrine effects of marijuana. J Clin Pharmacol. 2002;42:90S-96S.
[9] Liu X, Herbison AE. Dopamine regulation of gonadotropin-releasing hormone excitability in male and female mice. 20113;154O:340-50.
[10] Kolodny RC, et al. Depression of plasma testosterone levels after chronic intensive marihuana use. N Engl J Med. 1974;290:872-4.
[11] Gundersen TD, et al. Association between use of cannabis and male reproductive hormones and semen quality: a study among 1215 healthy young men. Am J Epidemiol. 2015;182:473-81.
[12] Velez ML, et al. Cannabis use disorders during perinatal period. In: cannabis use disorders. 2018:177-188.
