
By Dr. Tracy Tranchitella, ND
There it is again! That distinct flutter in your chest that kicks up your heart rate and leaves you feeling a bit breathless. It might feel as though your heart just skipped a beat or flip-flopped in your chest and you’re left wondering, “Did my body just take me on a little roller coaster ride or was that a heart palpitation?” For most women without underlying cardiovascular issues, the experience of a heart palpitation can range from a mild sensation to moderate discomfort, not because they are typically painful, but because they can make you acutely aware of your heartbeat.
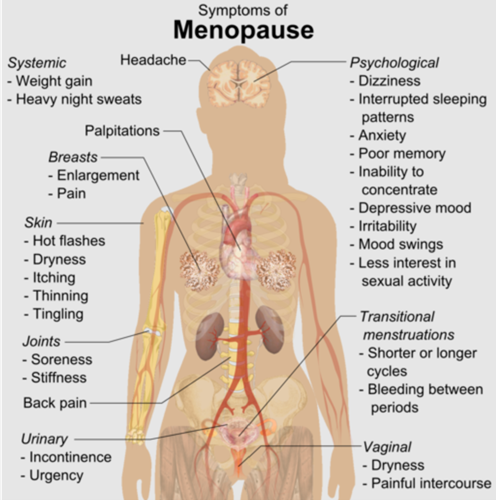
Heart palpitations can be associated with menopause, anxiety, hormonal fluctuations, hyperthyroidism, nutrient deficiencies, excessive caffeine, medications, mitral valve prolapse and heart arrhythmias. Heart palpitations are common and usually inconsequential. Although they can occur in the absence of heart disease, they may also be associated with a serious heart condition. If they are of new onset, occur frequently, and are associated with symptoms of dizziness, syncope, and pain, seeing your doctor for a complete evaluation is warranted.
Heart Palpitations and Hormones
Heart palpitations related to hormonal fluctuations can occur in women of all ages. Premenopausal women may experience heart palpitations during specific phases of their menstrual cycle when hormones are fluctuating. Pregnant women may also experience palpitations from rising hormones, increased blood volume and anemia. Heart palpitations in menopausal women occur from fluctuating and declining hormone levels.
Sex hormones can influence the rhythm of the heart by modifying ion channels that regulate electrical activity as well as regulating input from the autonomic nervous system (ANS). Menopause can be associated with a decrease in heart rate variability (HRV) due to either reduced parasympathetic or increased sympathetic outflow to the heart. Changes in electrical activity of the heart along with an increase in sympathetic tone, catecholamines (epinephrine or adrenaline, norepinephrine or noradrenaline) and cortisol can contribute to the development of heart palpitations.
What Is a Heart Palpitation?
A palpitation is a discernable change in cardiac rate or rhythm. There are four main physiological causes of palpitations:
- Extra-cardiac stimulation of the sympathetic nervous system (SNS), resulting in excess production of catecholamines and cortisol.
- Sympathetic overdrive, which may occur from stress, anxiety, panic disorder, hypoglycemia, and hypoxia.
- Increased circulatory volume, which may result in vasodilation and decreased blood pressure.
- Abnormal heart rhythms such as supraventricular tachycardia and atrial fibrillation, to name a few. Abnormal heart rhythms can range from mild to life-threatening and should always be treated appropriately.
Stressors and Midlife
Much of the medical literature on heart palpitations and hormones confirms that women in midlife and those entering menopause do experience palpitations. This seems to fall into the, “thanks for telling me what I already know” category. We know they’re happening, but why?
A deeper dive into the literature reveals some correlations that are not too surprising. More frequent and severe heart palpitations are associated with insomnia, a higher level of perceived stress, depression, and poor quality of life. Less physical activity, past or current smoking, and surgical versus natural menopause also contribute to increased frequency and severity of heart palpitations. Most of these correlates can be linked to a heightened stress response, and as mentioned above, heart palpitations can occur under increased SNS activity or activation of the stress response.
What makes our experience of stress during perimenopause and menopause different than our earlier years? What influences do estrogen and progesterone have on the stress response and the cardiovascular system that, without them, our hearts are a flutter – and not in a good way? Perhaps understanding the measurable effects of each hormone on heart rhythm is a good place to start.
Heart Rhythm and Hormones
A palpitation is experienced as a change in the rate and rhythm of the heart. Sex hormones can influence the rhythm of the heart in very distinct ways. As represented on an ECG, estrogen prolongs the QT interval while progesterone and testosterone shorten the QT interval. The QT interval represents the time it takes for the ventricles of the heart to contract and relax. On an ECG, the QT interval represents the electrical activity that occurs in the heart to generate a normal heartbeat. One QT interval is one heartbeat.
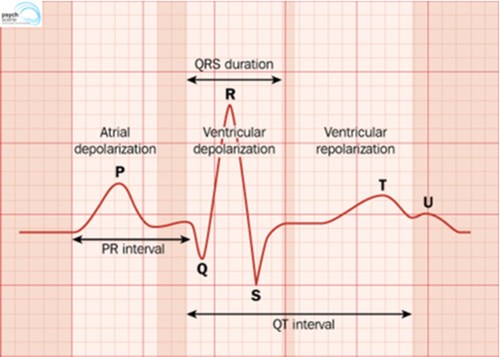
Relative ratios of estrogen and progesterone influence how the heart maintains a regular rate and rhythm. The individual effects of sex hormones tend to counterbalance each other via the expression and function of cardiac ion channels that regulate action potentials to coordinate a normal heartbeat. Cardiac myocytes have receptors for sex hormones whose activation can alter the electrical activity of the heart through modulation of ion channels that control the flow of sodium, potassium, and calcium.
Fluctuating hormone levels can lead to changes in the behavior and expression of myocardial ion channels and therefore interfere with a normal heartbeat. When hormones are balanced, the heart is less likely to experience an irregular rhythm in the presence of SNS stimulation or stress.
Sex Hormones and Cardiovascular Health
The effects of hormone replacement therapy (HRT) on cardiovascular outcomes in menopausal women can vary depending on the type of hormone used (synthetic versus bioidentical) and the route of delivery (oral, transdermal). Hormones are chemical messengers that regulate biological processes. The message that hormones deliver is based on their chemical structure. Synthetic hormones have a different structure than bioidentical hormones and may produce divergent effects within the cardiovascular system as compared to bioidentical hormones. For example, the use of oral forms of estrogen can be prothrombotic whereas the use of transdermal hormones does not seem to present with the same complication.
Estrogen tends to moderate stimulation of the heart and provides cardioprotective benefits in general. This is evidenced by the fact that premenopausal women have a decreased incidence of hypertension and cardiovascular disease as compared to men of the same age and women who are menopausal. Estrogen moderates blood pressure through three key mechanisms: dilation of blood vessels, inhibition of the renin-angiotensin system in the kidneys and moderation of SNS stimulation. Additionally, estrogen promotes cardiovascular health by reducing low-density lipoprotein, increasing high-density lipoprotein, improving glucose metabolism, decreasing insulin, protecting against atherosclerosis, and improving blood vessel response to injury.
The benefits of progesterone on cardiovascular health have not been as well studied as the benefits of estrogen. This may be due to the differing effects of synthetic progestins on cardiovascular health as compared to bioidentical or natural progesterone. Bioidentical progesterone has very different effects on the cardiovascular system as compared to synthetic progestins and tends to be associated with positive effects in both cardiovascular markers and overall function of the heart. Some of the cardiovascular benefits of bioidentical progesterone include decreased blood pressure, inhibition of coronary hyperactivity, and vasodilation. Bioidentical progesterone also has a natriuretic effect that reduces blood sodium levels, which in turn, can reduce blood pressure.
Sex Hormones, the SNS and the Stress Response
Both estrogen and progesterone are neurosteroids that act within the brain and nervous system, influencing biological functions and behavior. The main stress mechanism, the hypothalamic-pituitary-adrenal (HPA) axis and the SNS, interact with sex hormones in mediating the effects of stress. If sex hormones are fluctuating or have decreased altogether, their ability to moderate the stress response as well as regulate electrical signals within the heart is impaired. An increase in sympathetic tone and output coupled with less stable electrical activity within the heart can contribute to heart palpitations.
Much of the medical literature focuses on the drop in estrogen as a causative factor. In reference to the first two bullet points listed above regarding sympathetic tone, estrogen has the benefit of calming input into the SNS, which initiates the stress response. Estradiol and its metabolites, the catechol estrogens, appear to inhibit tyrosinase activity, which is an enzyme needed for the synthesis of norepinephrine.

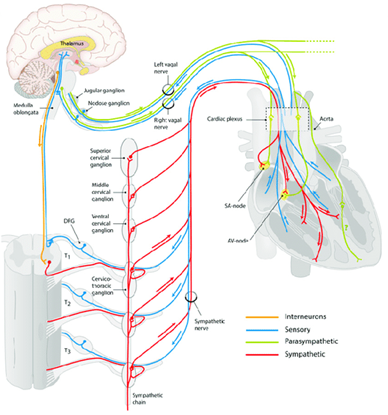
The presence of circulating estrogen creates a balance between the SNS responsible for the “fight or flight” response and the parasympathetic nervous system responsible for the “rest and digest” response.
Oophorectomized women demonstrated a decrease in HRV as compared to women of the same age who still had their ovaries. Decreased HRV indicates a decrease in parasympathetic tone or, in simple terms, less engagement of the branch of our ANS that promotes a sense of calm.
In postmenopausal women, estrogen therapy reportedly attenuates responses to mental stress rendering typically stressful events less stimulating to the SNS. In other words, we become more tolerant and better at managing stressful input. This is likely because estrogen moderates the release of norepinephrine, reducing activation of the HPA axis during a stressful event.
Studies on the effects of progesterone in the mid- and late luteal phase of the menstrual cycle show an increase in sympathetic nerve activity as measured by skin blood flow changes. Perhaps the higher levels of progesterone may be supportive of cortisol production as a means of providing negative feedback to inhibit continued production of norepinephrine from the SNS.
We need adequate cortisol to complete the loop of the stress response. Cortisol is a secondary responder whereas norepinephrine and epinephrine are the primary responders that initiate the physiological changes, which kick the body into action when under stress. Cortisol mobilizes energy to support that action but also tells the nervous system, “I’ll take it from here.”
Studies on the effects of progesterone on norepinephrine can be more telling. In animal models, injecting progesterone and corticosterone decreased norepinephrine and epinephrine. Metabolites of progesterone, particularly allopregnanolone, can have a calming effect on the brain and nervous system by potentiating the effects of gamma aminobutyric acid (GABA). GABA moderates the release of norepinephrine and epinephrine from the adrenal medulla thus lessening the initiation of the stress response within the adrenal glands.
In Summary
Heart palpitations in the perimenopausal woman can be related to changes in both estrogen and progesterone. This momentary irregular rhythm can occur in response to stimulation from the SNS in the presence of fluctuating and declining estrogen levels. Though progesterone plays a role in regulating mediators of the stress response, its distinct role in heart palpitations is less clear as it is not as well studied in its effects on the heart as estrogen. However, both estrogen and progesterone are necessary to regulate input to the SNS and are necessary to coordinate a normal heart rhythm.
Employing strategies that reduce stress, improve sleep, and balance fluctuating hormones can greatly improve heart palpitations. As a woman progresses into menopause, HRT may be her best option to address heart palpitations especially if they are frequent and bothersome. Sleep issues can be common during perimenopause and can add to the burden of stress that potentiates heart palpitations. If sleep is disrupted by hot flashes and heart palpitations are worse due to lack of sleep, hormone replacement might be the answer. Additionally, supplementing with a complete mineral complex, B vitamins and essential fats can provide the heart muscle with essential nutrients needed to maintain normal electrical activity.
Measuring Thyroid, Adrenal and Sex Hormones
ZRT offers a broad range of testing to assess sex hormones during all phases of a woman’s menstrual life. Estrogen, progesterone, and testosterone can be easily measured in saliva and dried blood spot (DBS). ZRT also offers dried urine testing that measures estrogen, progesterone metabolites, testosterone, cortisol, norepinephrine, and epinephrine, which provides a complete evaluation of sex hormones and stress response mediators. Ruling out thyroid dysfunction is often warranted with an irregular heart rhythm and ZRT offers a complete thyroid panel easily done at home through dried blood sampling. Saliva profiles can also provide a four-point measurement of cortisol to further assess the stress response. Additional cardiovascular markers, including blood lipids, fasting insulin and hsCRP, can be also conveniently measured in DBS.
Resources
Why does my heart feeling like it is doing hurdles? The Centre for Menstrual Cycle and Ovulation Research. 2013. Accessed May 30, 2022.
Wyss JM, Carlson SH. Effects of hormone replacement therapy on the sympathetic nervous system and blood pressure. Curr Hypertens Reps. 2002;5(3)3:241-246.
Hart EC, Charkoudian N, Miller VM. Sex, hormones and neuroeffector mechanisms. Acta Physiol (Oxf). 2011;203(1):155-165.
Sudhir K, Elser MD, Jennings EL, et al. Estrogen supplementation decreases norepinephrine-induced vasoconstriction and total body norepinephrine spillover in perimenopausal women. Hypertension. 1997;30(6):1538-1543.
Sedla T, Shufelt C, Iribarren C, et al. Sex hormones and the QT interval: a review. J Women’s Health (Larchmt). 2012;21(9):933-941.
Odening KE., Koren G. How do sex hormones modify arrhythmogenesis in long-QT syndrome? Sex hormone effects on arrhythmogenic substrate and triggered activity. Heart Rhythm. 2014;11(11):2107-2115.
Cersosimo MG, Benarroch EE. Estrogen actions in the nervous system: complexity and clinical implications. Neurology. 2015;85(3):263-273.
Costa S, Saguner AM, Gasperetti A, et al. The link between sex hormones and susceptibility to cardiac arrhythmias: from molecular basis to clinical implications. Front Cardiovasc Med. 2021;8:644279.
Placzek K. Feel awful at that time of the month? It’s more than just your hormones. TheZRT Laboratory Blog. Accessed May 30, 2022.
Smith A. The connection between GABA & sleep disturbances. TheZRT Laboratory Blog, Accessed May 30, 2022.
